Medicaid impact: IDD guide
Medicaid impact: IDD guide
Medicaid impact: IDD guide
Get clear, up-to-date insights on the 2025 Medicaid cuts and what they mean for IDD services. Learn what’s changing, how it could impact your agency, and what steps you can take to stay ahead. Enter your email to access the free guide.
Read a sneak peek



What’s changing in 2026
What’s changing in 2026
To respond effectively, agencies need to understand the current landscape. Medicaid remains the single largest payer for long-term services and supports (LTSS) for individuals with IDD—but it’s far from uniform. It encompasses a patchwork of state-administered waivers, reimbursement structures, and compliance requirements.
The federal cuts passed in 2025 have triggered a wave of changes across states. While some shifts may seem technical, they directly affect eligibility, billing timelines, audit readiness, and day-to-day care delivery. Staying ahead of these changes begins with understanding what has already gone into effect.
To respond effectively, agencies need to understand the current landscape. Medicaid remains the single largest payer for long-term services and supports (LTSS) for individuals with IDD—but it’s far from uniform. It encompasses a patchwork of state-administered waivers, reimbursement structures, and compliance requirements.
The federal cuts passed in 2025 have triggered a wave of changes across states. While some shifts may seem technical, they directly affect eligibility, billing timelines, audit readiness, and day-to-day care delivery. Staying ahead of these changes begins with understanding what has already gone into effect.
2025 Medicaid budget cuts: what’s now in effect
2025 Medicaid budget cuts: what’s now in effect
Congress has passed federal legislation reducing Medicaid spending by $1+ trillion over the next decade. Though the number is spread over 10 years, the impact is immediate. States are now receiving less federal funding, forcing them to stretch budgets, trim services, or adjust waiver policies.
Congress has passed federal legislation reducing Medicaid spending by $1+ trillion over the next decade. Though the number is spread over 10 years, the impact is immediate. States are now receiving less federal funding, forcing them to stretch budgets, trim services, or adjust waiver policies.
Federal funding reductions
The enacted cuts represent an estimated 11.8% drop in federal Medicaid funding to states. For many state Medicaid agencies already under strain, this has led to difficult decisions: capping services, limiting new waiver enrollments, freezing rates, or adjusting provider reimbursement. For agencies, that could mean delayed payments, tighter billing margins, and fewer approved hours for services already in place.
The enacted cuts represent an estimated 11.8% drop in federal Medicaid funding to states. For many state Medicaid agencies already under strain, this has led to difficult decisions: capping services, limiting new waiver enrollments, freezing rates, or adjusting provider reimbursement. For agencies, that could mean delayed payments, tighter billing margins, and fewer approved hours for services already in place.
Policy changes
In addition to funding cuts, the new law gives states expanded authority to reshape eligibility and service structures. Several key changes include:
- Mandatory work requirements for some adult Medicaid beneficiaries, creating risk of coverage loss for those unable to meet documentation requirements.
- Stricter redetermination protocols, which have already led to coverage loss for thousands—particularly among individuals with disabilities whose support networks must navigate complex paperwork.
- Greater flexibility in waiver redesign, allowing states to adjust what services are covered, how they’re billed, and what caps apply.
In addition to funding cuts, the new law gives states expanded authority to reshape eligibility and service structures. Several key changes include:
- Mandatory work requirements for some adult Medicaid beneficiaries, creating risk of coverage loss for those unable to meet documentation requirements.
- Stricter redetermination protocols, which have already led to coverage loss for thousands—particularly among individuals with disabilities whose support networks must navigate complex paperwork.
- Greater flexibility in waiver redesign, allowing states to adjust what services are covered, how they’re billed, and what caps apply.
Enter your email, and we’ll send you our the full eBook on projected Medicaid cuts.
Who is Giv?
Everything in one place.
Who is Giv?
Everything in one place.
Giv is designed to simplify your agency’s operations by streamlining Medicaid billing, complex scheduling, client documentation, and DSP payroll—all in one intuitive platform.
Giv is designed to simplify your agency’s operations by streamlining Medicaid billing, complex scheduling, client documentation, and DSP payroll—all in one intuitive platform.






Designed with care
Designed with care
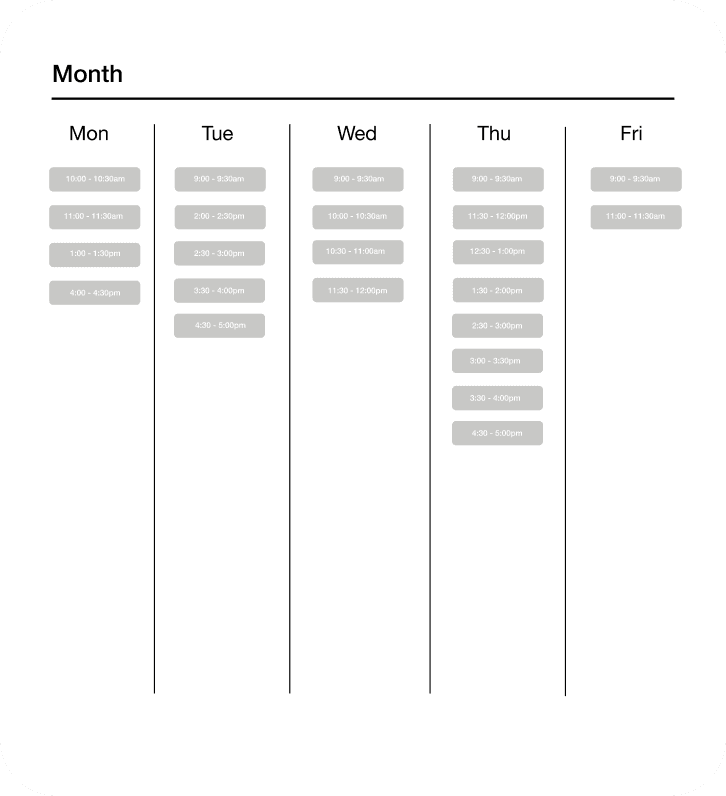
Easily schedule shifts for clients and staff. With the Giv mobile app, staff can clock in and out and manage the client services. Billing and payroll are handled automatically, making it easier than ever for you to focus on driving outcomes for clients.
Easily schedule shifts for clients and staff. With the Giv mobile app, staff can clock in and out and manage the client services. Billing and payroll are handled automatically, making it easier than ever for you to focus on driving outcomes for clients.
Person centered
Person centered
Our software is human-centered, tailored to drive outcomes for clients, empower staff, and automate agency owner tasks.
Our software is human-centered, tailored to drive outcomes for clients, empower staff, and automate agency owner tasks.
















Client Hub, EHR and eMAR.
Client Hub, EHR and eMAR.
Electronic health records and medication administration records combined and simplified to drive outcomes. Easily track every detail about your clients and empower your staff with critical information in real time through our mobile technology. Client outcomes are achieved when staff know what's required and can easily document every interaction.
Electronic health records and medication administration records combined and simplified to drive outcomes. Easily track every detail about your clients and empower your staff with critical information in real time through our mobile technology. Client outcomes are achieved when staff know what's required and can easily document every interaction.
Staff Hub, client care. Managed.
Staff Hub, client care. Managed.
Empower your direct support staff with everything they need to drive client outcomes. Timesheets, documentation and reporting are on autopilot, focusing your entire team on your clients needs. Easily track payroll and employee compliance documentation to always be audit ready.
Empower your direct support staff with everything they need to drive client outcomes. Timesheets, documentation and reporting are on autopilot, focusing your entire team on your clients needs. Easily track payroll and employee compliance documentation to always be audit ready.








Revenue Hub, your money, simplified.
Revenue Hub, your money, simplified.
Daily management of client billing and employee payroll is simplified when data flows directly from DSP interaction. Verify reported data without the manual calculation and entry. The revenue hub saves hours per week for your HR and billing teams.
Daily management of client billing and employee payroll is simplified when data flows directly from DSP interaction. Verify reported data without the manual calculation and entry. The revenue hub saves hours per week for your HR and billing teams.
Scheduling Hub,
intelligent shifts. Client info baked in.
Scheduling Hub,
intelligent shifts. Client info baked in.
Shifts that know your staff and clients are shifts that automate. Easily enforce client specific training for new direct support professionals, put goal tracking at the forefront and easily capture detailed client documentation. Your staff use one app, reducing their workload to focus them on clients.
Shifts that know your staff and clients are shifts that automate. Easily enforce client specific training for new direct support professionals, put goal tracking at the forefront and easily capture detailed client documentation. Your staff use one app, reducing their workload to focus them on clients.



FAQ



FAQ


FAQ